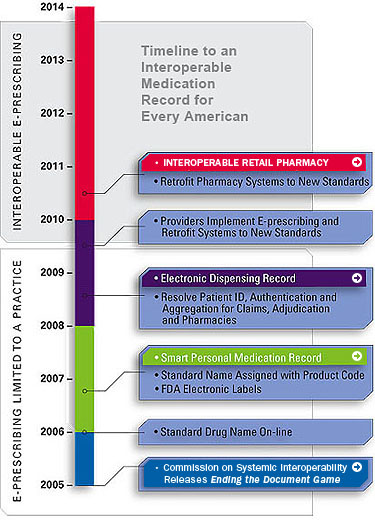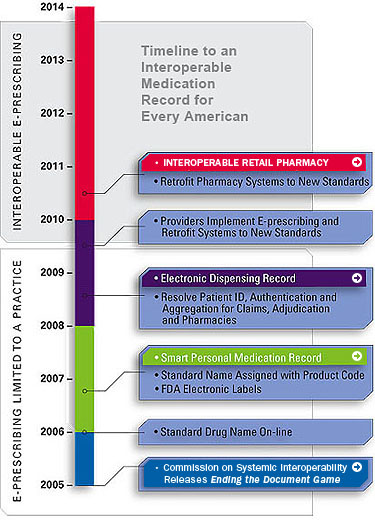
An interoperable medication record for every American
Having an electronic medication record for every American is a critical step toward achieving true interoperability in healthcare, giving treating physicians the information they need when they need it, allowing more effective care for their patients. It will bring all the medications an individual is currently taking to the doctor's attention at the time important decisions about new prescriptions are being made. With tens of millions of Americans relying on so many different medications to manage everything from elevated blood pressure to high cholesterol, a physician needs a patient's accurate and up-to-date medication list will allow a physician to prescribe the right medication at the right time for an individual's specific health concern, while avoiding the potentially harmful effects of a negative drug interaction.
Consider the following example of how one physician's practice might benefit from a patient's medication record.
2005: A portrait of today's state-of-the-art electronic medical record system
No Interoperability
Dr. Vivian Schilling wants to provide her patients with important information about their health. She also wants to have access to information that can help her be a better doctor. She uses an electronic medical record system in her office that allows her to access patient information from her desktop computer, tablet PC, handheld computer, or from home. Dr. Schilling is one of the 10 to 30 percent of more than 871,000 practicing physicians in the U.S. who is currently using a full version of electronic medical record system.
A unique user name and password securely connects Dr. Schilling to a patient's electronic "chart" right in her office, during a visit. While she talks to her patient, she enters information directly into the electronic medical record, documenting every detail of the case as the patient describes their symptoms and concerns. Dr. Schilling can do so without the potential problem of illegible handwriting since, depending on the device she uses, she can speak, type, or have her writing converted to text.
Each time Dr. Shilling sees a patient she reviews and updates the information in the electronic medical record. She also uses the system to view the results of imaging studies and laboratory tests she has ordered to help guide her treatment decisions. And as she determines the best course of care for her patient, the system provides another layer of safety by automatically presenting a series of alerts—potential concerns for a patient that the physician might wish to consider—based on the patient's age, sex, health condition and medication.
When Dr. Schilling chooses medication, she uses the system's pharmaceutical database, which contains thorough information about each of the drugs she could prescribe. With this tool, she can determine the appropriate prescription and avoid allergic reactions, unnecessary side effects and potentially harmful interactions between drugs.
The electronic medical record system also gives Dr. Shilling the ability to review all the patients she treats as a single group, so whenever new medication information is released she can quickly identify all the individuals taking a given medication and quickly provide them with important information that could impact their health. For example, when the U.S. Food and Drug Administration issued a Public Health Advisory about the withdrawal of Vioxx® from the American market, each of Dr. Schilling's patients who were taking Vioxx® were identified through the system and notified within 24 hours to stop taking the medication.
Dr. Schilling understands that patients who feel connected to her as their physician, and who are educated about their own individual health concerns, are more likely to be actively involved in the maintaining their health over time. They make better lifestyle choices, tend to eat better, watch their weight, and avoid significant health risks by getting enough exercise and by not smoking.
For example, when patient Betsy Clemmons arrives for her first office visit, Dr. Schilling invites her to enroll in a personalized online service that provides tools for health management. Describing the system as an "online connection to her own electronic medical record," Dr. Schilling tells Betsy about the things she will be able to do, including viewing information the doctor has entered in the electronic medical record about Betsy's health issues; reviewing information from past appointments, including any patient instructions the doctor recorded; receiving the results of tests almost as soon as they are released; requesting new appointments and prescription renewals; and receiving reminders about when her next health screening or tetanus shot is due—and all this will be available from any Internet connection, any time, day or night.
Perhaps most importantly, the tool contains links that provide Betsy with reliable information about the issues that matter most to her. For example, Betsy has a history of diabetes in her family. Since Dr. Schilling is ordering a blood glucose screening test at this first appointment, when Betsy gets home and logs in to the on-line tool, she can click on links to read in detail about diabetes, and better understand how she might avoid it, and see how others manage the disease. Of course, Betsy's personal information is encrypted and secure. No one but Betsy, Dr. Schilling, and the nursing and office staff directly involved in Betsy's care can access it.
Although the system significantly improves Dr. Schilling's ability to provide superior medical care, its effectiveness is limited because the information in it is limited to Dr. Schilling's practice. Ideally, a patient's vital medical information should be accessible to any physician treating that patient, no matter where the patient may be when care is needed. Still, Dr. Schilling's system is an important first step towards an interoperable medication record.
2006: Smart Personal Medication Record
Stage 1: Limited Interoperability
In 2006, Betsy becomes interested in having her own personal medication record. She wants to include prescriptions from all her physicians, along with over-the-counter medicines she takes on her own—not just prescriptions from Dr. Schilling.
Betsy finds a secure, password-protected online service that allows her to enter her medication history and access it at any time. She enters the medications she is currently taking, along with her known allergies, history of drug interactions, and other health conditions. All information will be entered manually by Betsy, but by entering the Federal Drug Administration's medication product code found on the label of her prescription bottles, official and complete drug information will be automatically linked to Betsy's record. With this, she can be alerted automatically if any of the drugs she is taking are recalled, no matter who prescribed them.
Betsy can grant access to her medication record to anyone she chooses, including physicians and family members. She can print out her medication history when going to a new physician, or print out a copy to keep in her wallet in case of an emergency.
The ability for consumers to have a personal medication record is a vital step toward an interoperable medication record. In this stage, anyone who has access to the Web will be able to access their own record 24 hours a day.
2008: Electronic Dispensing Record
Stage Two: Increased Interoperability
In 2008, the medication record becomes more connected to other physicians and information. When Betsy buys medication, the dispensing information is forwarded by the claims adjudicator or pharmacy to a secure clearing house. Betsy (and any provider she authorizes) can access this aggregate record of medications via a secure website. This automated electronic dispensing record replaces the smart personal medication record of 2006, described in the previous section.
Medicines are now recorded automatically in the record. Betsy doesn't have to remember to do it. All of her providers automatically see what each of them has prescribed. Whenever a medicine is dispensed it is checked for interactions with Betsy's allergies and with her other medicines. Full information about each medication, including dosing, side effects, interactions, lab conflicts, allergy alerts, disease contraindications, pricing, and drug image identification is still a click away with this electronic dispensing record. Notification about medication recalls is immediate and automatic.
At stage two interoperability, Betsy and each of her providers will be able to quickly and easily access all drug information as a single, aggregate record. However, the record is still not connected to practice-based e-prescribing systems. Dr. Schilling, and any other healthcare provider, must open a second display to manually check the aggregated record. During the prescribing process, automatic alerts are still limited to medications prescribed by that practice.
2010 and Beyond: Interoperable Medication Record
Stage Three: Complete Interoperability
In 2010, Dr. Schilling's office will have a fully interoperable medication record. The electronic medical record of 2005 has been retrofitted to use the standard drug names recognized by all systems. Over the last five years, all of Betsy's other providers have adopted standards-based e-prescribing systems. Providers and pharmacies instantly update each other on every change in medication information and prescriptions in real time. Finally, e-prescribing and dispensing are connected.
Dr. Schilling now has all the advantages of interoperability while maintaining the user-friendly electronic medical record interface of 2005. She can access patient records from home or in the office, allowing her to provide care for patients at any time. For example, when Betsy is admitted to the emergency room, Dr. Schilling as her primary care physician is able to connect to Betsy's information from her home. She sees both her outpatient medications and the IV solutions being used in the emergency room, and she gives a well-informed opinion of the treatment that should be taken.
Dr. Schilling's electronic medical record allows her to select medications from a drug information database that is updated automatically and at least on a daily basis. It includes direct links to all information in the electronic drug label.
With full interoperability now in place can prescribe medications and treat her patients using evidence-based guidelines, concise and easy-to-use clinical care guidelines based on the most updated and accurate medical information available.
For instance, Dr. Schilling often will use evidence-based guidelines in treating pneumonia, asthma, or sinusitis. Having this information available gives Dr Schilling the information needed to achieve a diagnosis, estimate a prognosis, choose the best therapy, determine potential harm, and provide the highest quality of care in a timely and efficient manner. Information is automatically tailored to avoid drug interactions and comply with the formulary (i.e. the list of medicines qualified for coverage) from the patient's insurer. With an interoperable medication record, the check for interactions is repeated at dispensing to catch changes in the patient's medication list since the prescription was first written.
By 2014, with Betsy's permission, de-identified (i.e., anonymous) abstracts of her medication record, lab tests and diagnoses are reported to a prescription reporting database for automated post-market surveillance. Bioinformatics algorithms check regularly for unexpected patterns to help identify safety concerns that might be missed by pre-marketing trials. These trials often exclude patients who may be at greater risk of certain adverse effects but will likely receive a drug when it is on the market. Pre-marketing trials that assess safety or efficacy also do not always detect relatively rare adverse events. Through interoperable electronic prescription reporting, the public has the best available tools for storing and analyzing safety reports and possible adverse drug events.
* * *
In 2010 and beyond, the benefits of a full interoperable medication record are realized. The building blocks of interoperability that were utilized in 2006, 2008, and 2010 provided the interface, framework, and content for the interoperable medication record. Dr. Schilling and Betsy can now have a better doctor-patient relationship by using all available information technology tools in an interoperable framework.